ISSN: 1308-5727 | E-ISSN: 1308-5735
Volume: 16 Issue: 2 - 2024
| 1. | Cover Pages I - IX |
| REVIEW | |
| 2. | Extensive Literature Review of 46,XX Newborns with Congenital Adrenal Hyperplasia and Severe Genital Masculinization: Should They Be Assigned and Reared Male? Tom Mazur, Jennifer ODonnell, Peter A. Lee doi: 10.4274/jcrpe.galenos.2023.2023-10-17 Pages 123 - 136 46,XX individuals born with severely masculinized genitals due to congenital adrenal hyperplasia (CAH) who have been assigned male at birth and reared male can successfully establish a male gender identity/role, find employment, marry, function sexually with a female partner, and develop positive mental health status. While there were a few individuals who reportedly did not fare well or who changed gender to female, the majority of those identifying as males appear to have an overall good quality of life. Parental/family support, along with the support of others, appears essential to a positive outcome as a male, or as a female. This paper suggests that serious consideration should be given to male gender assignment and rearing and, in certain situations, is justified. Disorders of sex differentiation teams should inform parents about the option for male assignment and rearing in 46,XX CAH infants with severe genital masculinization, which is a rare condition. To provide this option is concordant with the principles of ethics, transparency and with the Endocrine Society Guidelines and the American Academy of Pediatrics policy of fully informed consent. |
| ORIGINAL ARTICLE | |
| 3. | Screening of Mutations in Maturity-onset Diabetes of the Young-related Genes and RFX6 in Children with Autoantibody-negative Type 1 Diabetes Mellitus Enver Şimşek, Oğuz Çilingir, Tülay Şimşek, Sinem Kocagil, Ebru Erzurumluoğlu Gökalp, Meliha Demiral, Çiğdem Binay doi: 10.4274/jcrpe.galenos.2023.2023-5-10 Pages 137 - 145 INTRODUCTION: Maturity-onset diabetes of the young (MODY) is the most common type of monogenic diabetes. To date, mutations have been identified in 14 different genes of patients with a clinical diagnosis of MODY. This study screened mutations in 14 MODY-related genes and the regulator factor X6 (RFX6) gene in children. METHODS: The presence of clinical features of MODY and negative results for three autoantibody markers of type 1 diabetes mellitus (T1DM) in children and adolescents were used as inclusion criteria for genetic testing. The screening panel for next-generation sequencing included 14 MODY-related genes (GCK, HNF4A, HNF1A, HNF1B, PDX1, NEUROD1, KLF11, CEL, PAX4, INS, BLK, ABCC8, KCNJ11, and APPL1) and the RFX6 gene. RESULTS: Twenty-four different variants in MODY-related genes were identified in 49 children diagnosed with autoantibody-negative T1DM. Twelve variants were classified as pathogenic/likely pathogenic (P/LP) while 12 were interpreted as variant of unknown significance. Nine of the P/LP variants were found in GCK, two in HNF1B, and one in ABCC8. Three variants were novel, and one was a de novo variant. All but one of the variants exhibited heterozygotic inheritance. DISCUSSION AND CONCLUSION: The frequencies of the MODY subtypes differed from previous reports. Although GCK-MODY was the most frequent mutation in Turkish children, similar to previous studies, the second most prevalent MODY subtype was HNF1B-MODY. This study also established three additional novel mutations in different MODY genes. |
| 4. | Serum Ghrelin and Glucagon-like Peptide 1 Levels in Children with Prader-Willi and Bardet-Biedl Syndromes Doğa Türkkahraman, Suat Tekin, Merve Güllü, Güzin Aykal doi: 10.4274/jcrpe.galenos.2023.2023-7-7 Pages 146 - 150 INTRODUCTION: Prader-Willi syndrome (PWS) and Bardet-Biedl syndrome (BBS) are causes of pediatric syndromic obesity. We aimed to investigate a possible role for ghrelin and glucagon-like peptide-1 (GLP-1) in the pathophysiology of PWS and BBS. METHODS: The study included 12 children with PWS, 12 children with BBS, 13 pediatric obese controls (OC) and 12 pediatric lean controls (LC). Fasting serum ghrelin and GLP-1 levels were measured by ELISA. RESULTS: In the PWS group, no significant difference was detected for median ghrelin levels when compared with OC and LC, which were 0.96 (0.69-1.15), 0.92 (0.72-1.20) and 1.13 (0.84-1.29) ng/mL, respectively. Similarly, there was no difference in PWS median GLP-1 levels when compared with OC and LC; 1.86 (1.5-2.94), 2.24 (1.62-2.78) and 2.06 (1.8-3.41) ng/mL, respectively. In the BBS group, there was no difference in median ghrelin levels when compared with OC and LC; 1.05 (0.87-1.51), 0.92 (0.72-1.20) and 1.13 (0.84-1.29) ng/mL, respectively. Neither was there a significant difference in median GLP-1 levels; 2.46 (1.91-4.17), 2.24 (1.62-2.78) and 2.06 (1.8-3.41) ng/mL for BBS, OC and LC, respectively. DISCUSSION AND CONCLUSION: There were no differences in median fasting ghrelin or GLP-1 levels when comparing patients with PWS and BBS with obese or lean peers. However, similar studies with larger series are needed. |
| 5. | Associations of Adipocyte-derived Versican and Macrophage-derived Biglycan with Body Adipose Tissue and Hepatosteatosis in Obese Children Reyhan Deveci Sevim, Mustafa Gök, Özge Çevik, Ömer Erdoğan, Sebla Güneş, Tolga Ünüvar, Ahmet Anık doi: 10.4274/jcrpe.galenos.2024.2023-9-18 Pages 151 - 159 INTRODUCTION: In animal models of obesity, adipocyte-derived versican, and macrophage-derived biglycan play a crucial role in mediating adipose tissue inflammation. The aim was to investigate levels of versican and biglycan in obese children and any potential association with body adipose tissue and hepatosteatosis. METHODS: Serum levels of versican, biglycan, interleukin-6 (IL-6), and high sensitivity C-reactive protein (hsCRP) were measured by ELISA. Fat deposition in the liver, spleen, and subcutaneous adipose tissue was calculated using the IDEAL-IQ sequences in magnetic resonance images. Bioimpedance analysis was performed using the Tanita BC 418 MA device. RESULTS: The study included 36 obese and 30 healthy children. The age of obese children was 13.6 (7.5-17.9) years, while the age of normal weight children was 13.0 (7.2-17.9) years (p=0.693). Serum levels of versican, hsCRP, and IL-6 were higher in the obese group (p=0.044, p=0.039, p=0.024, respectively), while no significant difference was found in biglycan levels between the groups. There was a positive correlation between versican, biglycan, hsCRP, and IL-6 (r=0.381 p=0.002, r=0.281 p=0.036, rho=0.426 p=0.001, r=0.424 p=0.001, rho=0.305 p=0.017, rho=0.748 p<0.001, respectively). Magnetic resonance imaging revealed higher segmental and global hepatic steatosis in obese children. There was no relationship between hepatic fat content and versican, biglycan, IL-6, and hsCRP. Versican, biglycan, hsCRP, and IL-6 were not predictive of hepatosteatosis. Body fat percentage >32% provided a predictive sensitivity of 81.8% and a specificity of 70.5% for hepatosteatosis [area under the curve (AUC): 0.819, p<0.001]. Similarly, a body mass index standard deviation score >1.75 yielded a predictive sensitivity of 81.8% and a specificity of 69.8% for predicting hepatosteatosis (AUC: 0.789, p<0.001). DISCUSSION AND CONCLUSION: Obese children have higher levels of versican, hsCRP, and IL-6, and more fatty liver than their healthy peers. |
| 6. | Evaluating Postoperative Outcomes and Investigating the Usefulness of EU-TIRADS Scoring in Managing Pediatric Thyroid Nodules Bethesda 3 and 4 Aylin Kılınç Uğurlu, Abdurrahman Bitkay, Fatih Gürbüz, Esra Karakuş, Gülşah Bayram Ilıkan, Çağrı Damar, Seda Şahin, Merve Meryem Kıran, Nedim Gülaldi, Müjdem Nur Azılı, Emrah Şenel, İnci Ergürhan İlhan, Mehmet Boyraz doi: 10.4274/jcrpe.galenos.2024.2023-8-12 Pages 160 - 167 INTRODUCTION: The aim was to assess postoperative outcomes in pediatric thyroid nodules with atypia of undetermined significance (AUS/FLUS) or suspicious for a follicular neoplasm (SFN) and their respective the European-Thyroid Imaging Reporting and Data System (EU-TIRADS) scores. METHODS: Forty-four pediatric patients at a single center with thyroid nodules classified as AUS/FLUS or SFN from August 2019 to December 2022 were retrospectively reviewed. Data on demographics, thyroid function, nodule size, and ultrasonographic features were collected. Postoperative pathologies were categorized into benign, low-risk, and malignant neoplasms according to the World Health Organization 2022 criteria, and EU-TIRADS was used for retrospective radiological scoring. RESULTS: Among 21 (47.7%) of patients who had surgical intervention, 72% had Bethesda 3 and 28% had Bethesda 4 thyroid nodules. Post-surgical histopathological classifications were 43% benign, 19% low-risk, and 38% malignant. Of note, EU-TIRADS 3 and 5 scores were present in 44% and 56% of the benign cases, respectively. Malignant cases tended to produce higher EU-TIRADS scores, with 64% rated as EU-TIRADS 5. Bethesda category 4 nodules had a 66% malignancy rate, significantly higher than the 27% in category 3. DISCUSSION AND CONCLUSION: A substantial proportion of histologically benign cases were classified as EU-TIRADS 5, suggesting that EU-TIRADS may lead to unnecessary biopsies in benign cases. Malignant cases were more likely to have a higher EU-TIRADS score, indicating a positive correlation with malignancy risk, particularly in Bethesda 4 cases. However, the EU-TIRADS systems predictive value for malignancy in Bethesda 3 cases was poorer. |
| 7. | Microcephaly in Infants: A Retrospective Cohort Study from Turkey Gonca Keskindemirci, Öykü Özbörü Aşkan, Burak Selver, Alev Bakır Kayı, Gülbin Gökçay doi: 10.4274/jcrpe.galenos.2024.2023-5-3 Pages 168 - 176 INTRODUCTION: Microcephaly (MC) is a clinical finding mostly reflecting deficiency of brain growth. The aim of this retrospective cohort study was to assess risk factors and follow-up features of children with MC. METHODS: Childrens personal health records (n=7580) followed between 2002 and 2020 in the Unit of a Well Child Clinic were assessed retrospectively. The case group comprised children with MC. MC was defined as head circumference (HC) standard deviation score (SDS) value ≤-2 SDS. Age and sex-matched children with normal HC were selected as the control group. RESULTS: Children with MC (n=49) had more disadvantaged sociodemographic characteristics, such as young maternal and paternal age and low maternal and paternal education. Breastfeeding was more common among controls (n=98). Resolution of MC was observed in 26 (53.1%) children with MC, whether it was mild (HC SDS between -2 and -2.9) or severe (HC SDS ≤3). Children with persistent MC had poorer developmental milestones than controls and cases with resolution. Sociodemographic features or developmental milestones in mild and severe MC did not differ. DISCUSSION AND CONCLUSION: These results suggest that the use of a definition of MC of ≤-2 SDS would be appropriate in order not to miss cases on follow-up. Greater sociodemographic equality may prevent some cases of MC. Further studies are needed evaluating socioeconomic factors on MC. |
| 8. | Assessment of Executive Function Skills in Children with Isolated Growth Hormone Deficiency: A Cross-sectional Study Gülsüm Yitik Tonkaz, Atilla Çayır doi: 10.4274/jcrpe.galenos.2024.2023-10-6 Pages 177 - 184 INTRODUCTION: The aim of this study was to evaluate executive function (EF), such as inhibition and working memory, in children with isolated growth hormone deficiency (IGHD) using performance-based tests and parent-report scales. METHODS: A total of seventy children between the ages of 7 and 12 years were included in the study. Half (n=35) had children with IGHD and half were healthy controls. To evaluate the EF performances of the participants, the Visual Aural Digit Span Test-B Form (VADS-B) and Stroop task were applied. EF was also evaluated using the Behavior Rating Inventory of Executive Function (BRIEF). RESULTS: Children with IGHD scored lower on the VADS-B form for short-term memory (p<0.05) compared to healthy controls. In addition, the completion time for the Stroop-color/word test was significantly longer in children with IGHD (p<0.05). For children with IGHD, their parents reported higher scores on all sub-scales of the BRIEF scale, with statistically significant differences for all sub-scales with the exception of organization of materials (p<0.05). DISCUSSION AND CONCLUSION: In this study, children with IGHD had poorer EF skills compared to unaffected peers. EF skills may influence academic success by affecting childrens language skills, mathematical comprehension, cognitive flexibility, and hypothetical thinking. We believe that psychiatric evaluation of children with IGHD before and during treatment may positively contribute to both their academic performance and social relationships. |
| 9. | Salivary Sex Steroid Levels in Infants and the Relation with Infantile Colic Fulya Mete Kalaycı, Özlem Gürsoy Doruk, İbrahim Mert Erbaş, Osman Tolga İnce, Makbule Neslişah Tan, Adem Aydın, Ayhan Abacı, Ece Böber, Korcan Demir doi: 10.4274/jcrpe.galenos.2024.2023-11-2 Pages 185 - 191 INTRODUCTION: The hypothalamic-pituitary-gonadal axis is active during minipuberty, the timing of which coincides with infantile colic. To the best of our knowledge, the relationship between these entities has not been previously investigated. METHODS: Saliva samples were collected from 15- to 60-day-old term infants (n=139) between 9 am and 5 pm. Group 1 included infants with infantile colic (n=68, 54.4% female) while the remaining healthy infants constituted Group 2 (n=71, 47.9% female). Salivary levels of estradiol (Esal) in females and testosterone (Tsal) in males were measured by ELISA in duplicate. RESULTS: The median (25th-75th centile) age and birth week for all infants were 33 (29-43) days and 39 (38.1-40) weeks, respectively. Levels of Tsal in males [Group 1, 73.35 (59.94-117.82) pg/mL vs Group 2, 77.66 (56.49-110.08) pg/mL, p=0.956] and Esal in females [Group 1, 3.91 (2.76-5.31) pg/mL vs Group 2, 4.03 (1.63-12.1) pg/mL, p=0.683] were similar. However, in subjects with infantile colic (Group 1), Esal and body mass index (BMI) standard deviation scores of females were slightly correlated (Group 1, rs= 0.393, p=0.016 vs. Group 2, rs= 0.308, p=0.076) and there was a significant correlation between the sampling time and Tsal in males (Group 1, rs= 0.469, p=0.009 vs. Group 2, rs= -0.005, p=0.976). DISCUSSION AND CONCLUSION: Random salivary sex steroid levels were similar in infants with and without infantile colic. However, in subjects with infantile colic, Esal levels in females were positively correlated with BMI and Tsal levels were higher later in the day among males. Thus, sex steroid production may be altered during minipuberty in subjects with infantile colic. |
| 10. | Non-thyroidal Illness in Children with Congestive Heart Failure Biswajit Sahoo, Aashima Dabas, Binita Goswami, Anurag Agarwal, Sumod Kurian doi: 10.4274/jcrpe.galenos.2024.2023-12-7 Pages 192 - 199 INTRODUCTION: To estimate the proportion and risk factors of non-thyroidal illness (NTI) in children with congenital heart disease (CHD) with congestive heart failure (CHF). METHODS: This study enrolled children (6 weeks to 60 months age) with CHD and CHF. The clinical profile and disease severity, derived from the Pediatric Early Warning Score (PEWS) was recorded. Baseline blood samples were taken within 24 hours of hospitalization and evaluated for free tri-iodothyronine (fT3), free thyroxine (fT4), thyroid stimulating hormone (TSH), N-terminal pro-brain natriuretic peptide (NT pro-BNP) and reverse T3. RESULTS: A total of 80 (64 acyanotic CHD) children of median (interquartile range) age 5 (2.5, 8.0) months were enrolled. NTI was seen in 37 (46%) of whom 27 had low fT3 levels. The proportion of NTI was highest in children with severe disease (20/30), than moderate (4/9) or mild disease (13/41) (p=0.018). Ten (27%) patients with NTI died compared to 2 (4.7%) without NTI with unadjusted odds ratio (OR) [95% confidence interval (CI)] 7.593 (1.54, 37.38); p=0.006. After adjusting for NTI, shock and NT-pro-BNP levels, PEWS was the only significant predictor of mortality (OR: 1.41, 95% CI: 1.03, 1.92; p=0.032). Linear regression for fT3 identified a significant relationship with log NT-BNP [beta -3.541, (95% CI: -1.387, -0.388)] and with TSH [beta 2.652 (95% CI: 0.054, 0.383)]. The cutoff (area under the curve, 95% CI) that predicted mortality were fT4 <14.5 pmol/L (0.737, 0.60, 0.88), fT3/rT3 index <1.86 pg/ng (0.284, 0.129, 0.438) and NT pro-BNP >3725 pg/mL (0.702; 0.53, 0.88). DISCUSSION AND CONCLUSION: NTI was present in a significant proportion of children with CHD and CHF. fT3 level was significantly associated with NTBNP levels and thus severity of CHF. |
| CASE REPORT | |
| 11. | Juvenile Granulosa Cell Tumor Mimicking HAIR-AN in a 4-year-old: A Case Report Rachel Choe Kim, Ilya Goldberg, Trevor Van Brunt, Hamama Tul-Bushra, Rebecca Batiste, Andrew H. Lane, Helen Hsieh doi: 10.4274/jcrpe.galenos.2022.2022-4-17 Pages 200 - 204 Predominantly androgen secreting juvenile granulosa cell tumors (JGCT) are uncommon and few reports have been published. We present a case of a JGCT that presented with signs of prepubertal hyperandrogenism and insulin resistance to highlight the possible interaction between hyperandrogenemia and hyperinsulinism. A 4-year-old girl presented with acanthosis nigricans and hyperinsulinism, mimicking the hyperandrogenism, insulin resistance and acanthosis nigricans syndrome at an age much younger than is typical for this diagnosis. Laboratory studies revealed elevated insulin, inhibin A and B, and total testosterone. All laboratory results normalized after unilateral salpingo-oophorectomy. The final diagnosis was Stage 1A JGCT. This case highlights the importance of including ovarian tumors in the differential diagnosis when considering causes of virilization and insulin resistance. This case also suggests a potential relationship between excess testosterone secretion and hyperinsulinemia and strengthens evidence that hyperandrogenemia may promote hyperinsulinism in ovarian disease. |
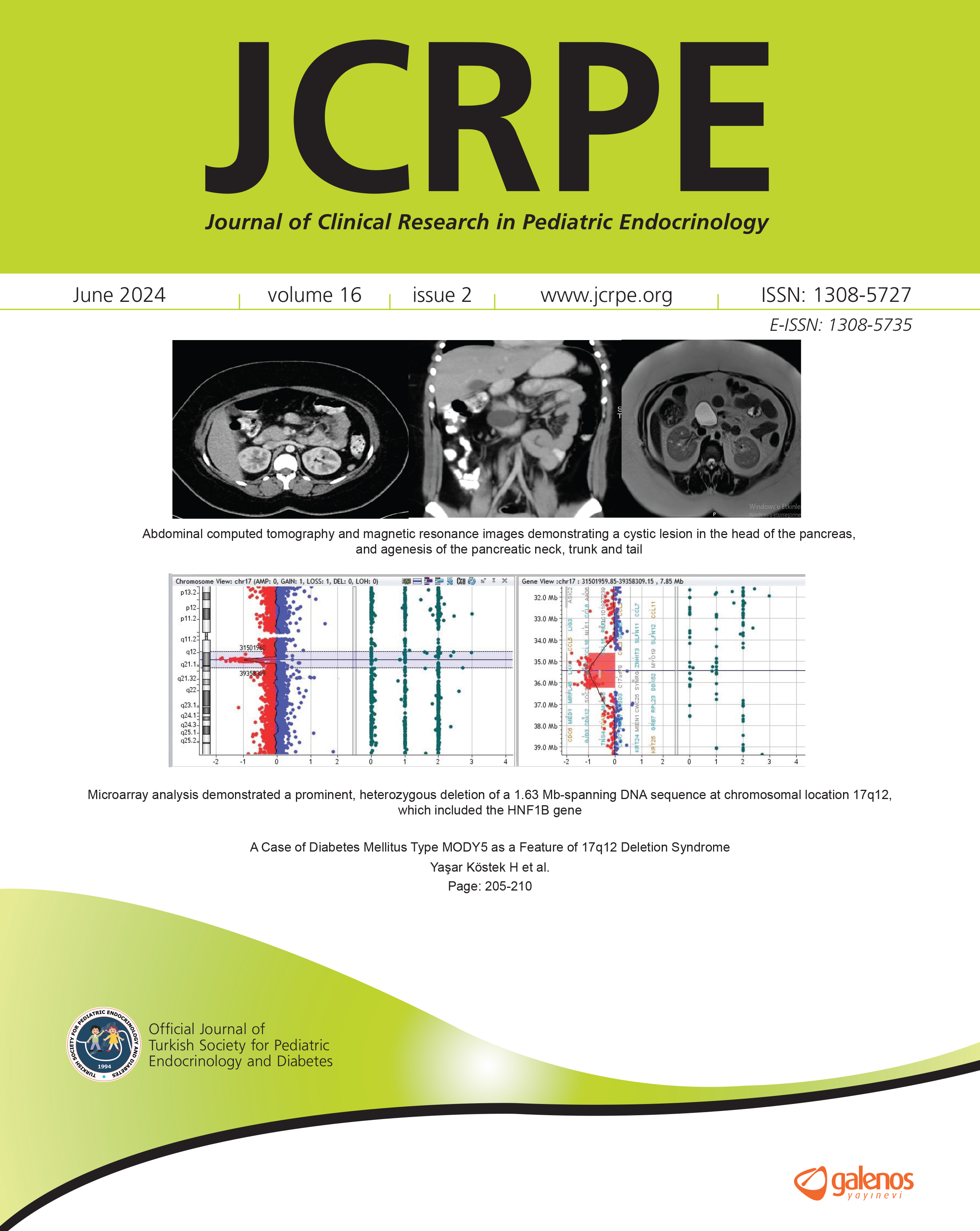
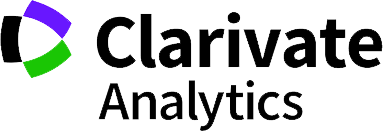
| 12. | A Case of Diabetes Mellitus Type MODY5 as a Feature of 17q12 Deletion Syndrome Hümeyra Yaşar Köstek, Fatma Özgüç Çömlek, Hakan Gürkan, Emine Neşe Özkayın, Filiz Tütüncüler Kökenli doi: 10.4274/jcrpe.galenos.2022.2022-3-2 Pages 205 - 210 Maturity onset diabetes of the young (MODY) is characterized by noninsulin-dependent diabetes diagnosed before the age of 25 years with an autosomal dominant inheritance. Rare mutations in the hepatocyte nuclear factor-1-beta (HNF1B) gene produce a syndrome that resembles MODY. About half of patients diagnosed with MODY type 5 due to HNF1B variants, carry a whole gene deletion, known as 17q12 deletion syndrome. 17q12 deletion syndrome is a rare chromosomal anomaly and is typified by deletion of more than 15 genes, including HNF1B resulting in kidney abnormalities and renal cysts, a diabetes syndrome and neurodevelopmental or neuropsychiatric disorders. A 12-year-old girl was referred after high blood sugar was detected in the hospital where she presented with polyuria and polydipsia, which had persisted for one month. Her serum magnesium (Mg) level was low at 1.5 mg/dL (normal value 1.6-2.6) and glycated hemoglobin was 14% (normal value 3.6-5.8) concurrent with a c-peptide of 1.54 ng/mL (normal value 0.8-4). MODY5 was suspected but the NGS gene panel (ABCC8, BLK, CEL, GCK, HNF1A, HNF1B, HNF4A, INS, KCNJ11, KLF11, NEURODD1, PAX4, PDX1, RFX6, ZFP57, GLIS3, FOXP3, NEUROG3, G6PC2) did not identify any abnormality. During follow-up, her serum Mg remained low (1.2 mg/dL) together with elevated urinary Mg excretion at 172.5 mg/day. An HNF1B variant was again suspected in a patient with chronic hypomagnesemia with normal basal C peptide level. Abdominal computed tomography and magnetic resonance imaging revealed a 43 mm diameter, cystic lesion in the head of the pancreas, with agenesis of the pancreatic neck, trunk and tail. Genetic testing using a microarray analysis was subsequently performed and a heterozygous deletion at 17q12, including HNF1B, was detected. In case of clinical suspicion of HNF1B variants, further genetic examination using other techniques such as MLPA and CGH array may be required to detect the variant. This is because deletions and duplications may not be detected using next generation screening panel techniques. |
| 13. | Endocrine Evaluation and Homeostatic Model Assessment in Patients with Cornelia de Lange Syndrome Ángela Ascaso, Ana Latorre-Pellicer, Beatriz Puisac, Laura Trujillano, María Arnedo, Ilaria Parenti, Elena Llorente, Juan José Puente-Lanzarote, Ángel Matute-Llorente, Ariadna Ayerza-Casas, Frank J. Kaiser, Feliciano J. Ramos, Juan Pié Juste, Gloria Bueno-Lozano doi: 10.4274/jcrpe.galenos.2022.2022-4-14 Pages 211 - 217 The aim of this study was to expand knowledge about endocrine disorders in individuals with Cornelia de Lange syndrome (CdLS), a rare developmental genetic disorder with anomalies in multiple organs and systems. Hormone levels, clinical scores, anthropometric measurements, and molecular analysis were assessed in 24 individuals with CdLS. Hyperprolactinemia was the most common endocrine disorder. Three patients showed subclinical hypothyroidism. Concerning the gonadotropic axis, mildly delayed puberty was observed, as well as genital anomalies, such as cryptorchidism. Despite short stature, levels of insulin-like growth factor 1 and insulin-like growth factor-binding protein 3 tended to be normal. Three prepubertal individuals without risk factors had higher than normal values for the homeostatic model assessment of insulin resistance (HOMA-IR) and for insulinemia, suggesting insulin resistance. Furthermore, two adults had elevated body mass indexes associated with HOMA-IR values over the cut-off values. CdLS may lead to dysregulation of the endocrine system, particularly in patients with high HOMA-IR values and insulinemia who are at risk of insulin resistance. Therefore, clinical follow-up with comprehensive hormonal assessment appears warranted in individuals with CdLS. |
| 14. | Stress Induced Hyperglycemia in Early Childhood as a Clue for the Diagnosis of NEUROD1-MODY Nur Berna Çelik, Naz Güleray Lafcı, Şenay Savaş-Erdeve, Semra Çetinkaya doi: 10.4274/jcrpe.galenos.2022.2022-6-15 Pages 218 - 223 Maturity-onset diabetes of young MODY type 6 is a rare form of monogenic diabetes caused by mutations in neuronal differentiation 1 (NEUROD1). Clinical features vary in a large spectrum in terms of age and body mass index (BMI) at diagnosis. Here, we reported the youngest patient with a NEUROD1 variant to the best of our knowledge. A 2.1-year-old girl was referred to pediatric endocrinology clinic for elevated fasting BG (104 mg/dL) which was detected at another center where she had been evaluated for loss of appetite. Her maternal aunt and uncle had been diagnosed with type 2 diabetes mellitus (DM) at the age of 40 and 45 years; they were obese (BMI: 30.2 and 30.6 kg/m2). At the age of 3.7 years old, she was hospitalized for buccal cellulitis and plasma glucose concentration was 239 mg/dL at admission. Targeted next-generation sequencing (NGS) was performed considering the stress induced hyperglycemia without serious illness, negative islet cell antibodies and insulin autoantibodies, age at the presentation, and family history of DM. NGS analysis revealed a previously reported heterozygous missense variant in NEUROD1. Segregation studies showed that the identified variant was inherited from her 44-year-old mother with a BMI of 27.2 kg/m2 and a normal oral glucose tolerance test. Heterozygous NEUROD1 mutations cause low-penetrant diabetes that is heterogeneous in terms of clinical features as some patients fulfill the classic MODY definition and others are mimicking type 2 DM. Clinical manifestations and family history should be carefully evaluated in patients with stress induced hyperglycemia to identify candidate cases for molecular testing, and proper follow-up should be initiated in affected individuals. |
| 15. | Successful Management of Severe Hypercalcemia with Zoledronic Acid: A Report of Two Pediatric Cases Fatih Kilci, Jeremy Huw Jones, Filiz Mine Çizmecioğlu-Jones doi: 10.4274/jcrpe.galenos.2022.2022-9-3 Pages 224 - 228 Severe hypercalcemia associated with vitamin D intoxication or malignancy in children is a rare and life-threatening condition. There is little published experience with Zoledronic acid (ZA) in the treatment of pediatric severe hypercalcemia. Here, we present two pediatric cases of severe hypercalcemia, one due to vitamin D intoxication and the second to malignancy, in which ZA was used as the first-line bisphosphonate in the treatment. While both cases responded well to a single dose of ZA, the second case experienced hypocalcemia requiring calcium treatment after ZA infusion. Our report shows that ZA may be an effective option in the treatment of severe pediatric hypercalcemia, although patients should be followed closely after infusion due to the risk of hypocalcemia. We provide additional published evidence for the effectiveness of ZA in correcting severe pediatric hypercalcemia and hope this will encourage future studies with larger numbers of patients. |
| 16. | Severe Growth Hormone Deficiency in an Indian Boy Caused by a Novel 6 kb Homozygous Deletion Spanning the GH1 Gene Basma Haris, Idris Mohammed, Umm Kulthum Umlai, Diksha Shirodkar, Khalid Hussain doi: 10.4274/jcrpe.galenos.2022.2022-5-9 Pages 229 - 234 Growth disorders resulting in extreme short stature (ESS) are often a result of deficiency in growth hormone (GH) released from the pituitary gland or a defective GH releasing receptor. Genetic defects in the GH1 and GHRHR genes account for around 11.1-20% of ESS cases, resulting in a rare condition called isolated GH deficiency (IGHD). We describe the characterization of a GH1 genetic defect discovered in a 3-year-old male patient with ESS, developmental failure and undetectable serum levels of GH. There was a family history of short stature, with both parents being short. Whole genome sequencing of the patient DNA revealed a large, novel 6 kb homozygous deletion spanning the entire GH1 gene in the patient. While the deletion was homozygous in the proband, it was present in the heterozygous state in the parents. Thus, we report a novel homozygous deletion including the GH1 gene leading to IGHD-type 1A associated with ESS. |
| 17. | Short Adult Height After Rapid-tempo Puberty: When is it too Late to Treat? Peter A. Lee doi: 10.4274/jcrpe.galenos.2024.2024-1-13 Pages 235 - 242 A rarely reported phenomenon of rapid-tempo puberty in which the physical changes of puberty and testosterone levels increase very rapidly has not been reported outside apart from in two reviews. The resulting rapid advancement of skeletal age causes early completion of growth with shorter adult stature than expected. This appears to be genetic given its occurrence in the present report in two families, one with three brothers, one with two. We also describe potential treatments and found for the youngest that early initiation of standard therapy preserved or reclaimed adult height (AH) potential. The foreshortened AH in this situation involves rapidly advancing puberty resulting from high circulating testosterone levels leading to rapid advance in skeletal age. This was recognized earlier among younger brothers and treatment with gonadotropin-releasing analogues, growth hormone (GH) and/or aromatase inhibitor therapy (AIT) was tried. Two brothers in family A and family B were treated. Case 5 started treatment early enough so his AH was within target height (mid-parental height) range. Cases 2, 3, 4 were tried on GH and/or AIT with outcomes suggesting benefit. The prevalence and mechanism of rapid-tempo puberty requires further study. Furthermore, as illustrated by two of the current cases, this phenomenon may have a heightened prevalence, or at least may occur, in children previously diagnosed with constitutional delay of growth, underscoring the need to be cautious in assurance of a normal AH outcomes in this population, based on data from a single assessment. |
| LETTER TO THE EDITOR | |
| 18. | Vitamin D Receptor Gene Polymorphisms with Type 1 Diabetes Risk: Correspondence Hinpetch Daungsupawong, Viroj Wiwanitkit doi: 10.4274/jcrpe.galenos.2023.2023-9-8 Page 243 Abstract | |
| 19. | In response to: Letter to: Vitamin D Receptor Gene Polymorphisms with Type 1 Diabetes Risk: Correspondence Ramasamy Thirunavukkarasu, Ayyappan Chitra, Arthur Asirvatham, Mariakuttikan Jayalakshmi doi: 10.4274/jcrpe.galenos.2024.2024-5-13 Page 244 Abstract | |